Skin Cancer
Skin cancer is a dangerous and potentially fatal condition that affects millions of people each year. Those who live active lives and enjoy spending time outdoors are especially prone to skin cancer due to the damage that prolonged sun exposure and harmful UV rays can cause. Thankfully, however, skin cancer is often curable, especially when diagnosed and treated early. As a board-certified plastic surgeon, Dr. Antell can surgically remove cancerous growths using specialized techniques that maintain your appearance, while also ensuring your health and safety.
Dr. Darrick E. Antell: Skin cancer treatment in NYC
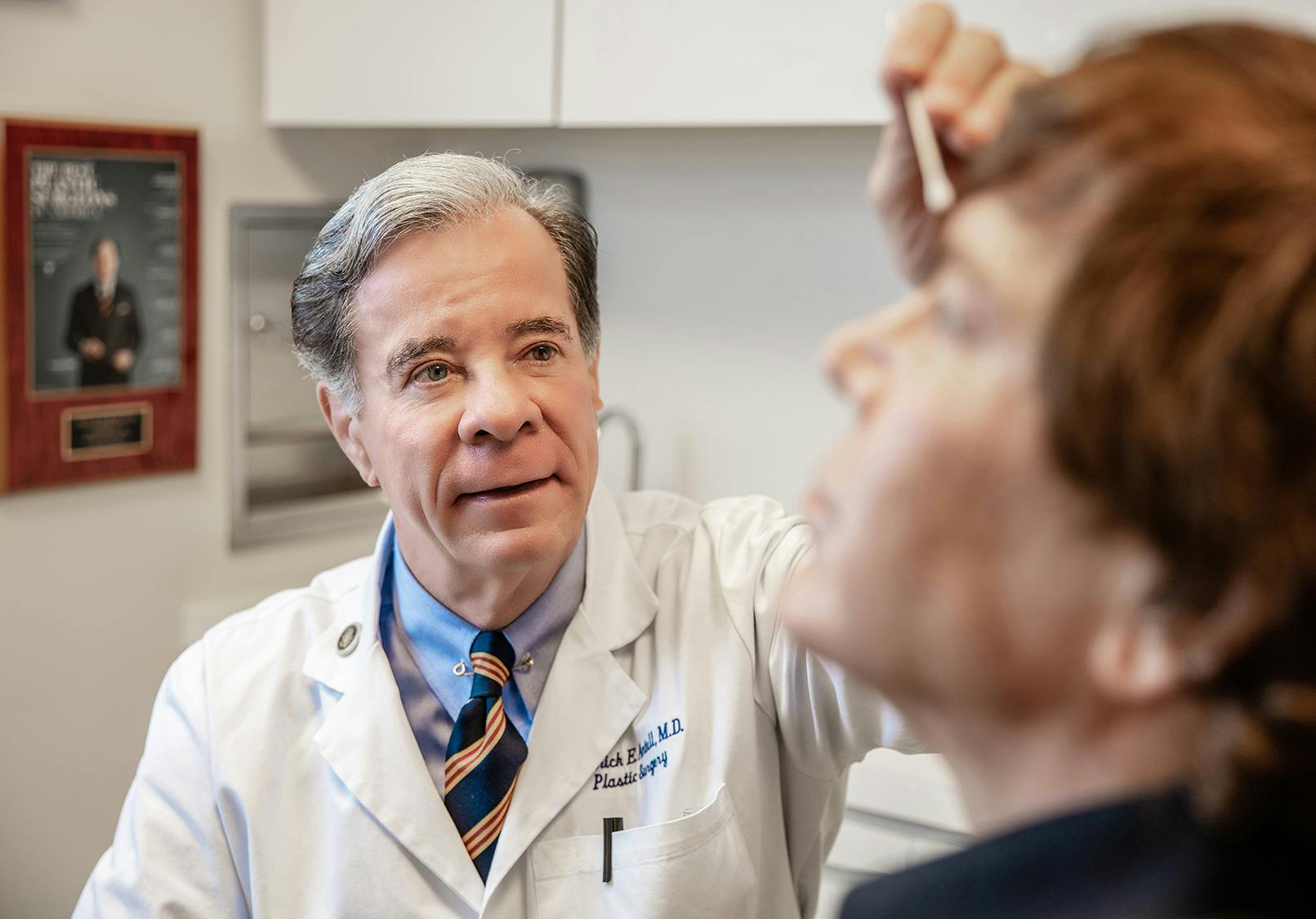
Dr. Darrick E. Antell, M.D., F.A.C.S, is a renowned plastic surgeon dedicated to providing comprehensive solutions for the aesthetic and medical issues associated with skin cancer. Regarded as one of the most talented plastic surgeons practicing in the New York area, Dr. Antell has achieved acclaim for his work, both from his peers and his patients. Over the course of his illustrious career, he has repeatedly been named a “Top Plastic Surgeon” by Harper’s Bazaar, Town and Country, Vogue, and New York Magazine. With the core philosophy that “plastic surgery should whisper, not scream,” Dr. Antell strives to perform complex surgeries with minimal evidence that any work was done.

Due to his groundbreaking research on the effects of sun, stress, and smoking on the aging process in identical twins, he is an expert on the damaging effects that excessive sun can have on the skin. His private, state-of-the-art facility, as well as his high level of personalized care, has resulted in celebrities, politicians, and discerning patients who demand private and professional care seeking his services for their skin cancer treatment in NYC.
What is skin cancer?
Skin cancer is a condition in which the skin cells begin to multiply uncontrollably, causing visible and often painful lesions that can be fatal if not diagnosed and treated as soon as possible. This type of cancer occurs as a result of damage to the DNA of the skin, resulting in mutations as the cells reproduce. Although skin cancer is most common in skin that is often exposed to sunlight, such as the face, neck, and hands, it can occur anywhere on the body.
There are three common types of skin cancer:
Basal cell carcinoma (BCC)
Basal cell carcinoma is a form of skin cancer that arises from the skin’s basal cells in the outermost layer of the skin. Basal cells are often referred to as the skin’s “reproductive” cells, as they play an important role in the regeneration of new skin cells. The appearance of BCCs differs for each individual but can often look like an open sore, pink/red growth, or shiny bump. The most common form of skin cancer, BCCs usually appear on parts of your skin that are the most exposed to the sun. Due to the slow growth of BCCs, they are highly curable and cause minimal damage when treated early.
Squamous cell carcinoma (SCC)
Squamous cell carcinoma is a form of skin cancer that arises from the skin’s squamous cells in the outermost layer of the skin. Although different for each individual, SCCs can sometimes appear as a scaly red patch, open sore, or wart-like growth. Long-term exposure to UV radiation from the sun and tanning beds is the most typical cause of SCCs and, as a result, they are most often found on areas that are most exposed to the sun and show signs of sun damage, such as wrinkles and age spots. The second most common form of skin cancer, SCCs can grow rapidly and metastasize if not detected early.
Melanoma
Melanoma is a form of skin cancer that arises from melanocytes, the skin cells that produce melanin pigment (which gives skin its color). Often resembling moles, melanomas can be found on any area of the body, even those that are not routinely exposed to the sun. It is often caused by intense sun exposure, such as that which results in sunburn, and tanning bed use. Melanoma is the most dangerous of the three most common types of skin cancer due to its ability to metastasize rapidly. However, with early detection and skin cancer treatment in Manhattan, it can be cured.
How is skin cancer diagnosed?
Although most skin lesions are non-cancerous, due to his dedication to ensuring the safety and well-being of each patient, Dr. Antell sends out samples of any biopsied, shaved, or excised lesion to a lab for evaluation. At the lab, a pathologist thoroughly tests and examines the specimin to determine the presence of any suspicious cells. Based on these findings, Dr. Antell will proceed with the appropriate treatment, including removing any cancerous skin cells if indicated or referring you to an oncology specialist.
How is skin cancer treated?
The treatment of your suspicious growth will depend on its size and location, as well as the type of cancer and its stage of growth, if already determined. However, in many cases, the first step is to remove the growth. At Dr. Antell’s private office and operating room, this procedure can often be performed the same day as your initial consultation using local anesthesia. His goal will be to remove the growth in a way that ensures your safety, while also producing a pleasing appearance - a consideration that may be especially important if the growth is in a highly visible area.
How is skin cancer removed?
The options for skin cancer treatment in NYC include:
- Excision of the growth
- Radiation therapy
- Cryosurgery (freezing the cancer cells)
- Topical chemotherapy, in which anticancer drugs are applied to the skin
- Mohs surgery (a procedure in which the tissue is removed layer by layer and immediately examined under a microscope)
What if my cancer has spread?
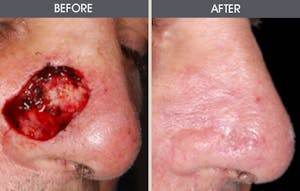
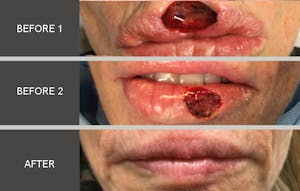
If the cancer is more extensive or has spread to your lymph nodes or elsewhere in the body, a more complex treatment plan may be required. The different techniques used in treating skin cancers can be life-saving, but they may leave a patient with less than pleasing cosmetic or functional results. Fortunately, in addition to his extensive experience treating skin cancer, Dr. Antell is also an expert in performing reconstructive procedures to restore your appearance following skin cancer removal.
Will my skin cancer treatment leave a scar?
Dr. Antell offers his patients the most advanced techniques for skin cancer removal and reconstruction to restore a natural appearance. A scar is inevitable, although it is a small price to pay for removing the cancerous growth from your body and preventing further damage. With decades of experience, meticulous surgical techniques, and the utmost dedication to his patients, Dr. Antell’s expertise will ensure that the scar is as inconspicuous as possible.
How can I prevent my skin cancer from recurring?
You can limit the risk of further skin cancer growths by:
- Avoiding prolonged exposure to the sun, especially between 10 AM and 4PM and during the summer months
- Wearing protective clothing such as wide-brimmed hats and long sleeves when you know you will be out in the sun
- Using a broad-spectrum sunscreen with an SPF of at least 15 every day
- Using a water-resistant, broad-spectrum sunscreen with an SPF of at least 30 when participating in extended outdoor activities
- Applying sunscreen liberally 30 minutes before going outside and re-applying it every two hours and after swimming or sweating
- Examining your skin regularly for changes and new growths and seeing a physician at least once a year for a professional skin exam
- Contacting a qualified doctor, such as Dr. Antell, immediately if you notice any suspicious growths
Skin Cancer Reconstruction Before & Afters
How do I get started with my skin cancer treatment?
Dr. Antell’s state-of-the-art practice on Park Avenue in the Upper East Side of New York City offers the most modern and innovative skin cancer treatments. If you have any concerns about a skin growth, meet with Dr. Antell for a thorough examination of your condition, as well as a recommendation for the best treatment to address both medical and cosmetic concerns. Contact us today at (212) 988-4040 to schedule your consultation and get started.